What are the benefits of using a Dexcom G6 or Freestyle Libre Continuous Glucose Monitor (CGM) to manage your Type 1 or Type 2 Diabetes? As an insulin-dependent T2D, I am always looking for new or better ways to manage my diabetes and learn about how my body manages the carbohydrates I consume.
I have been using a CGM to manage my diabetes since the fall of 2018. Here are some of my observations of the benefits of using a Continuous Glucose Monitor (CGM) from the perspective of an insulin-dependent Type-2 diabetic.
REMINDER: This information and website is not intended to provide any medical advice, opinion, or decision making, and cannot replace or be a substitute for your relationship with your healthcare provider.
Table of Contents
- What is a Continuous Glucose Monitor (CGM) for diabetes?
- How does a CGM read (blood) glucose?
- How many times a day do you test your blood glucose?
- The relationship between the number of times you glucose and better A1c results
- A CGM will help us understand how our blood glucose reacts to the foods we eat
- CGM can help support Diabetes Biohacking
- Help Warn of you Severe Hypoglycemia
- Automated Insulin Delivery for Type 1 Diabetics through Looping and CGM
- Final Thoughts
What is a Continuous Glucose Monitor (CGM) for diabetes?
A Continuous Glucose Monitor or CGM is a medical device that continuously checks the glucose in your body every 5 to 15 minutes, all day and all night. A CGM allows you to monitor your glucose day and night without the need for traditional blood glucose finger tests. A CGM also allows you to see the trends and patterns in your glucose to help you and your diabetes team make more informed treatment decisions. Different CGM devices collect information in different manners using tiny sensors. In some cases, the sensor is placed under the skin of your belly in a quick and painless fashion, however, a CGM typically adheres to the back of your arm or your belly for 10 to 14 days.

The picture to the right is me wearing my 14 days Freestyle Libre CGM sensor. You can read more about my thoughts on the Libre here. I also have a series of questions and answers about the FreeStyle Libre that are very much applicable to all CGM systems.
Four of the most common CGM’s on the market are the Dexcom G6, Abbott Freestyle Libre, Medtronic Guardian Connect CGM and Eversense (this one intrigues me). However, not all CGM’S are available in every country as they are subject to approval by your federal health / drug administrations as approved treatments for diabetes. Within Canada, both the Dexcom G6 and Freestyle Libre are available as approved diabetic devices and are covered by most public and private health insurance; although in most cases there is a requirement to be on insulin.
How does a CGM read (blood) glucose?
The technology used by each CGM is slightly different. However, unlike traditional finger blood glucose tests that use a sample of your blood to test for the amount of glucose in your body, a Continuous Glucose Monitor typically reads your glucose from your interstitial fluids below your skin.
Interstitial fluid (IF), or simply tissue fluid, is a mixture of water, ions, and small solutes that are forced out of the blood plasma by the systolic pressure created when the heart pumps. Plasma is a mixture of water and many other constituents, which carry blood cells and oxygen to various parts of the body. I look at IF, as the fluid that sits beneath our skin. As if is born from our blood, it carries our glucose and is read by the CGM. Hint: CGM’s work best when we are well hydrated.
Here is a great info-graphic that shows how typical CGM sensors interact with the interstitial fluid and the glucose travelling in your blood.

Source: http://www.medtronicdiabetes.com/
There are 1,440 minutes in a day? How many times a day do you test your blood glucose?
There are 1,440 minutes in a day? How many times do you test your glucose? Can you really say how well you know what your blood sugars are doing?
To be conservative let’s say as a typical diabetic we test our blood glucose with finger tests five times a day – a fasting glucose test when we wake up, before breakfast, lunch, and dinner and before our correction dose at bedtime. Presuming each test is a 1-minute snapshot of our glucose levels, that is less than 1% of the total minutes in a day or 5 minutes of testing? What are your blood sugars doing the other 23 hours and 55 minutes (1,435 minutes)? Even if you tested your glucose 10 times a day with a finger test, besides our poor fingers feeling like a pin cushion, we still have huge gaps in our glucose trends. This is where your continuous glucose monitor truly shines.
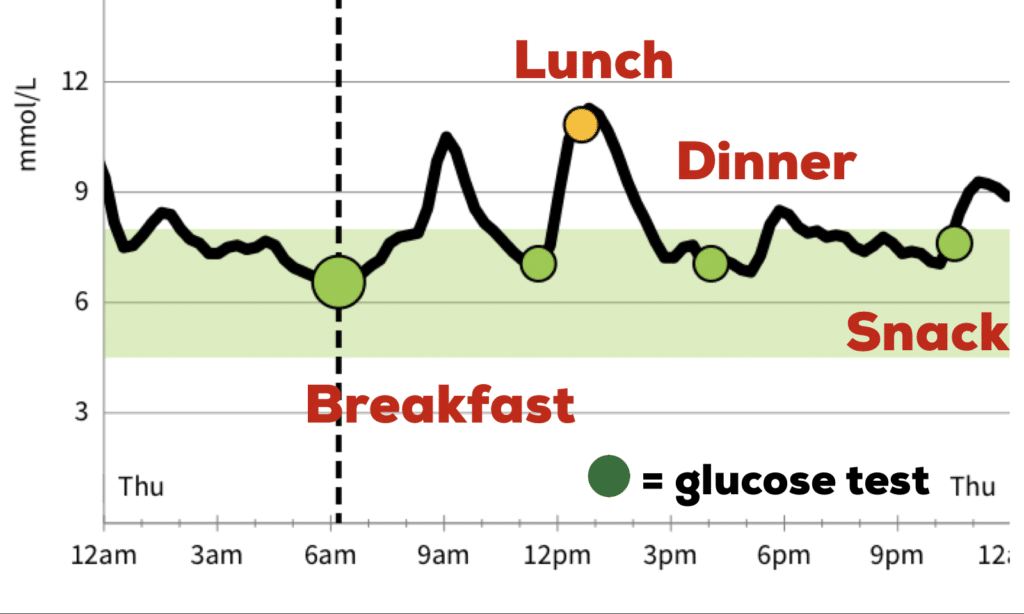
A typical CGM tests your glucose every five minutes or 288 times a day. Using our same 5 traditional finger blood glucose tests, that still accounts for only 2% of the day. With a CGM, you now have the ability to track and monitoring your glucose up to 24 hours a day as you can see below in the black trend line.
Studies have shown that there is a positive relationship between testing your glucose and better A1c results
Did you know that studies have shown that the more often a diabetic test their blood glucose the better their diabetes management? A 2013 study published by Diabetes Care (iv) showed that the higher number of blood glucose measurements per day was strongly associated with a lower HbA1c level. Results from the study suggest that if you test your blood glucose 2 times a day, your A1C is usually around 9%. Diabetics that test the blood glucose more than 10 times reduce their A1c to closer to 7%.

Imagine the successes you can have with your glucose control if you CGM tests your blood glucose 288 times a day? A similar study by 50,000 CGM readers worldwide suggests that the typical CGM user scans their sensors / checks their CGM readers 16 times a day can drop their HbA1C to less that 7% [Blue Graph]. More importantly, the events in minutes per day of Hypoglycemia falls by 40% in high vs infrequent testers (v) [Red Graph].

A CGM will help us understand how high, how quickly and how long our blood glucose reacts to the foods we eat
A CGM will help us understand how high, how quickly and how long our blood glucose reacts to the foods we eat. Looking at the image above, you can see the spikes in my blood sugar with each meal (breakfast, lunch, and dinner) and the spread or gap between the start of the spike and the end of the rise, for how long it took my T2D body to return back to “normaL”. You can also see the benefits of better carbohydrate and balanced meal consumption with a smaller spike at dinner. You can also see my not so great snack around 10:30 at night. The dots were where I took a specific glucose reading.
From the insights gained from our CGM, we can that how our Type 2 bodies can manage certain foods will be different for all of us depending on how much “natural” glucose control we have. Do you know what foods work better with your diabetes than others? If for no other reason, I truly believe this is one of the main reasons why EVERY diabetic should wear a Continuous Glucose Monitor, even for a short 10 to 14 day period between diabetes clinic visits. This includes both Type 1 and Type 2 diabetics on insulin as well as Type 2 diabetics that are managing their diabetes with pills, diet, and exercise.
Imagine as recently diagnosed Type 2 diabetic, for a 10 to 14 day period, the power of keeping a food log and being able to see EXACTLY:
- How high did my blood sugars rise with certain foods
- How quickly did my blood sugars climb, and did they return back to the normal range?
- How long did my blood sugars stay above 10 mmol/L (180 mg/dL) after I ate?
Do your sugars rise with everything you ate? Are your sugars increasing as they naturally would with food, and coming back down to a normal 5 or 6; or are they following a steady staircase as the day progresses, coming down but not as much as they increased, eventually leaving you in the high teens or twenties by bedtime? How well do certain types of food work together? What works better? FOOD X, or FOOD X and Y? How good or bad is that “diabetes” friendly snack?
The successes with diabetes management are as much about learning as they are about good habits.
CGM can help support Diabetes Biohacking
Biohacking is the practice of examining and changing our body chemistry, in the case of Type 2 diabetes, our bodies’ ability to self-manage glucose, through food science and self-experimentation. CGM is a critical tool in diabetes biohacking. What do you consider your gold standard of glucose management? For me, through a balanced diet (carbohydrates, fibre, and the glycemic index of foods, and medication), how well can I get my T2D body mimic the glycemic response of a typical or healthy adult?
What is a typical glycemic response to food?
What is the typical bodies’ response to a controlled oral glucose tolerance test (OGTT) or incremental glucose peak (IGP)? For the OGTT test, you will then be asked to drink a liquid containing a certain amount of glucose (usually 75 grams). Your blood will be taken again every 30 to 60 minutes after you drink the solution to measure how high, and for how long your glucose remains in your blood.
We are all aware of how our bodies “should” work. We consume carbohydrates, cells in your pancreas (known as beta cells) are signalled to release insulin into your bloodstream. Insulin then attaches to and signals cells to absorb sugar from the bloodstream. Insulin is often described as a “key,” which unlocks the cell to allow sugar to enter the cell and be used for energy. (i) How much sugar (glucose) in our blood; after 2 hours; is an indication of glycemic control or diabetes.
The OGTT tests how well our bodies respond to the sugar drink. In other words, you drink the sugar drink, your sugars rise. Your body releases insulin and over the next two yours, the insulin helps your body convert the glucose to energy until your glucose levels return to a normal range between 3.9 and 7.1 mmol/L (70 to 130 mg/dL). Depending on the results of OGTT, we are diagnosed with diabetes.
What is your diabetes diagnosis: Normal Fasting glucose is typically 3.3 to 5.5 mmol/L (60 to 100 mg/dL) and after 2 hours of the glucose tolerance test, a blood glucose less than 7.8 mmol/L (140 mg/dL). In contrast, a pre-diabetic or someone with impaired glucose tolerance have an OGTT of A 2-hour value between 7.8 and 11.1 mmol/L (140 and 200 mg/dL). We are diagnosed with Type 2 diabetes with a 2-hour OGTT value of 11.1 mmol/L (200 mg/dL) or higher.
What does this mean for a Type 2 Diabetic?
As Type 2 diabetics, how well our bodies can manage our glucose varies depending on how extensively our disease has progressed. In the early stages of a typical Type 2 diagnosis, we can improve our glycemic control through a better diet (don’t consume as many carbohydrates) and exercise (force our bodies to use more carbohydrates). As our disease progresses, oral medications are used to improve our glycemic control, eventually progressing to a lifestyle similar to a Type 1 Diabetic, where Insulin is required to replace the insulin our pancreas would normally produce.
Why is this important to recognize? The severity of our Type 2 Diabetes, directly relates to how well our body can manage glucose, and more importantly how that relates to the foods we eat. The same meal consumed by one Type 2 Diabetic and how well we can use the carbohydrates in that food, will be completely different for each of us. More importantly, how much glucose is left in our bodies between meals will be very accordingly. This is where bioHacking and our CGM’s shine.

Source: https://instagram.com/p/B8b0eyRoHc0/
Preliminary published by the American Diabetes Association (ii) found that when vegetables and protein were eaten before carbohydrates, there were a reduction om glucose levels by as much as 37%, compared to when carbohydrates were consumed first. More recently, research has suggested that the extent of the glucose-lowering effect of protein and fat was found to be even greater when they are consumed before carbohydrates than mixed with them (iii). Give it a try and let us know what you observe with your CGM? How bad for your sugars are your favourite bowl of cereal? How bad is that All You Can Eat (AYCE) Susi (Check out my IG Post) (ADD LINK)
CGM’s Can Help Warn of you Severe Hypoglycemia or HyperGlycemia Events’
How well do you know when your blood sugars (glucose) are getting out of control? Are they getting dangerously high, are they too low to safely drive or at risk of a hypoglycemia event? A continuous glucose monitor can work to warn you or your caregivers when your glucose is getting out of range. CGM’s like the Dexcom G6 can work with your mobile phone, to continuously communicate with your mobile phone (about once every five minutes) via a Bluetooth connection to notify you if your glucose is above or below a defined threshold. The FreeStyle Libre, with the assistance of a 3rd party receiver to read the Near Field Communications of the Libre such as the Ambrosia NightRider BluCon and MiaoMiao that can read the sensor every 5 minutes and send the data via Bluetooth to an app which then notifies you of approaching highs or lows.
Although neither device is perfect, for example, your phone needs to be on and charged, your phone needs to be within the Bluetooth range of the sensor, and the app needs to be continuously running. However, this opens up some incredible opportunities. Despite these imperfections – something that could never be achieved with finger tests alone.
CGM’s are Opening the Doors for Automated Insulin Delivery for Type 1 Diabetics
Unlike Type 2 Diabetics whose pancreases and use of insulin are not as efficient as they need to be, Type 1 Diabetics do not produce insulin naturally and rely on doses of insulin with each meal to allow their bodies to manage their carbohydrate intake and fuel their bodies. Many T1D’s have migrated taking individual doses of insulin with each meal to the convenience of using an insulin pump to manage their insulin dosing.
An insulin pump constantly gives you a small amount of insulin, called a “basal rate,” throughout the day and night to help control your blood sugar. When you need extra insulin to cover a meal or to correct high blood sugar, you tell the pump to give you a small dose of rapid-acting insulin. Similar to a CGM saving your fingers from daily glucose tests, an insulin pump saves a diabetic from routine insulin infections, limiting them to a single catheter needle every two or three days. To date, insulin pumps are not “smart”, they are simply an easy delivery method for daily insulin use.
This is where the magic of CGM, an insulin pump, and a “highly experimental and not an approved therapy treatment for diabetes”, called Looping start to play well together.
Looping is highly experimental. You take full responsibility for building and running this system and do so at your own risk.
So What is Insulin Looping?
Loop is an app template for building an automated insulin delivery system. Loop works much like an artificial pancreas. Using your CGM, the loop system knows what your glucose levels are at any given time. Have you been exercising and your sugars are lower, did you just participate in an AYCE Sushi lunch and they are spiking higher than estimated, or were on the go and just could not eat as well as we normally do. An insulin pump requires manual adjustments to balance these needs. With Looping, the changes are seamless – with your CGM, working with the looping framework / application to then adjust the amount of insulin automatically depending on your glucose level – aka an artificial pancreas. Imagine a diabetic world where blood sugars are close to normal, without the concerns of hypoglycemia or hyperglycemia occurrences?
Although looping is not at the point where it is a mainstream diabetes solution – it does open the doors for where this blending of technologies will take us over the next generation of insulin pumps and continuous glucose monitors.
My thoughts about Continuous Glucose Monitoring for Type 2 Diabetics
Continuous Glucose Monitors are a game-changer for diabetes education and management. The simplicity and convenience of tap and scan to download the last 8 hours of readings from you Freestyle Libre or the Bluetooth connection to your mobile device with the Dexcom G6 has a direct relationship with patient responsibility and accountability to their diabetes management. Most of us are very visual learners, while others are still in denial as to the extent our bodies are no capable to manage carbohydrates on their own. I would be the first to admit, I Have tested my body time and time again, to see if just this year, things are improving on the diabetes front not continuing to slide towards insulin dependence.
A few days into using a CGM for the first time, a user in a diabetes FaceBook group I participate in enthusiastically wrote, ” I’ve been using Libre for a few days, blown away by how easy it is, how convenient, it’s a joy to test now! Doctor didn’t want to prescribe it to me as he felt it was just for type 1 diabetics .. doctors need an education about how easy these things are to use and how they can benefit anyone that is diabetic. “

Being able to see, how high did my blood sugars rise with certain foods, how quickly did my blood sugars climb, and did they return back to the normal range, and how long did my blood sugars stay above 10 mmol/L (180 mg/dL) after I ate are important lessons for any Type 2 diabetic. I strongly believe for that reason alone, insurance companies should be funding the use of CGM on a short term basis. Why not make them part of your diabetic equipment annual maximum for any non-insulin dependent Type 2? The long term benefits of proper diabetes care are well known and documented.
REFERENCES
- (i) What is Insulin? – http://endocrineweb.com/conditions/type-1-diabetes/what-insulin on 2020-02-12
- (ii) Food Order Has a Significant Impact on Postprandial Glucose and Insulin Levels, Alpana P. Shukla, Radu G. Iliescu, Catherine E. Thomas, Louis J. Aronne, Diabetes Care. 2015 Jul; 38(7): e98–e99.
- (iii) Impact of Nutrient Type and Sequence on Glucose Tolerance: Physiological Insights and Therapeutic Implications Lorenzo Nesti, Alessandro Mengozzi, Domenico TricòFront Endocrinol (Lausanne) 2019; 10: 144. Published online 2019 Mar 8. doi: 10.3389/fendo.2019.00144PMCID: PMC6418004
- (iv) Evidence of a Strong Association Between Frequency of Self-Monitoring of Blood Glucose and Hemoglobin A1c Levels in T1D Exchange Clinic Registry Participants. Kellee M. Miller, MPH1⇑, Roy W. Beck, MD, PHD1, Richard M. Bergenstal, MD2, Robin S. Goland, MD3, Michael J. Haller, MD4, Janet B. McGill, MD5, Henry Rodriguez, MD6, Jill H. Simmons, MD7, Irl B. Hirsch, MD8, for the T1D Exchange Clinic Network in Diabetes Care 2013 Jul; 36(7): 2009-2014. https://doi.org/10.2337/dc12-1770
- (v) Real-world flash glucose monitoring patterns and associations between self-monitoring frequency and glycaemic measures: A European analysis of over 60 million glucose tests. Timothy C. Dunn, Yongjin Xu, Gary Hayter, Ramzi A. Ajjan https://doi.org/10.1016/j.diabres.2017.12.015

