Being diagnosed with one chronic disease is not necessarily enough. Here is my story about being diagnosed with Type 2 diabetes (T2D) in addition to my Crohn’s disease and how I manage the two chronic diseases.
As Crohn’s suffers; patients; the lucky few (or is it really that few); or however we choose to label ourselves, life has certainly drawn us a short straw. Although I have to admit, the rapid weight loss can be a great way to get back into that fun outfit buried deep in your wardrobe, however, even that is short-lived after a few weeks of Prednisone munchies. The truth of the matter is that as Crohnies we cherish good quality toilet paper and always know where the closest washroom is. We have a chronic disease, Crohn’s for life – isn’t that enough for one person to have to deal with? The trouble is, unfortunately not!
Do you have a chronic disease? Check out our survey on diabetes, IBD, Crohn’s and colitis – go to the survey here or in the sidebar.
Diagnosed with Type 2 Diabetes
If you do a quick Google search on “Crohn’s and diabetes (Type 1 or Type 2)” about 1,150,000 results are found. Comparatively, a search for Chicken Gumbo soup stirs up about 257,000. With numbers like these, maybe an association between Type 2 or T2 Diabetes and Crohn’s Disease is not that uncommon after all. For many of you who have read my history please bear with me – I promise I will be brief.
I was first diagnosed with Crohn’s disease in 2005 (age 33). I would not say that my disease ever went into remission but for a while, I did live drug-free – although I am positive my gastroenterologist would have scolded me. Late last fall I started to experience persistent chest pains. Like most guys, stubborn as we are, I kept putting it off. I suppose I am still gun-shy from years of Doctors telling me that my digestive issues were “all in my head”, and to try to get another bizarre diagnosis or feel like I am wasting a doctors time is not my favourite past time. By late November, the pains had increased to a point that on my way home one evening I made a detour to the local emergency department. 12 hours later I was sent home with a “clean bill of health” (albeit with the pains persisting). A few hours later the emergency department called, noting that further review of my blood work showed that my blood sugar levels were elevated (11.9 mmol/L or 215 mg/dl for my U.S. friends) and to follow with my family doctor.
The question that went through my head at the time was simply this, “Was being in the emergency department, enough to get everyone’s heart pumping and adrenaline flowing. No wonder my sugars were high!” Denial, right? Like a good patient, over the next few weeks I met with my family doctor going over the various test results – it was confirmed, “Delayed Fasting Glucose” or “Prediabetes”.
What is prediabetes?
Well the Public Health Agency of Canada describes prediabetes as:
PRE-DIABETES MEANS THAT YOUR BLOOD GLUCOSE LEVELS ARE HIGHER THAN NORMAL, BUT LOWER THAN IF YOU HAVE TYPE 2 DIABETES. PRE-DIABETES IS ALSO CALLED IMPAIRED GLUCOSE TOLERANCE OR IMPAIRED FASTING GLUCOSE.
IF YOU HAVE BEEN DIAGNOSED WITH PRE-DIABETES, THEN YOU HAVE AN INCREASED RISK FOR DEVELOPING TYPE 2 DIABETES.
Over the coming months, my fasting glucose levels (collected after an 8 to 10 hour fast) were bouncing all around the board – 6.8, 9.1 – enough was enough. It looked like, pre-diabetics education and a few lifestyle changes were in order. Education/knowledge is power after all, right?
I have to commend the South Lake Regional Health Centre on excellent diabetes education, support program and staffing. Although I admit, the cohort in the pre-diabetes class was a little skewed towards the retired and me at 38 just didn’t fit in. Regardless, the day-long course I attended in late January provided an overview of “Diabetes” and more importantly how to not to be one of the 4 out of 10 people in the class whose disease would progress to Type 2 Diabetes.
Exercise, diet, portion size, managed carbohydrate intake was to become my new norm, and fibre became my next best friend. Ok – lets put on the breaks a little – did he just say fibre? Sounds easy enough! However, when we had a little training session in the class on how to your a glucometer, I know I was in trouble – at the end of the training the nurse did a little roll-call on what our blood-sugar levels were – 4.5, 5, 6.5 – I don’t recall anyone being above 7.0 – that was until they came to me – 9.9 (anything under 10.0 two hours after a meal is considered normal). Only thing the diabetes education nurse emphasized in the class was that if through good diet, and exercised, It could take years for someone to progress from prediabetes to diabetes – in my case, the years were more like months as you can see in the chart.

As of March 18th, 2010, I was officially diagnosed with Type-2 Diabetes. Chronic illness number two! WOOT! UGG!
What is Type-2 Diabetes
Diabetes Canada defines Type 2 diabetes as a disease in which your pancreas does not produce enough insulin, or your body does not properly use the insulin it makes. As a result, glucose (sugar) builds up in your blood instead of being used for energy. Your body gets glucose from foods like bread, potatoes, rice, pasta, milk and fruit. To use this glucose, your body needs insulin. Insulin is a hormone that helps your body to control the level of glucose in your blood. High blood glucose levels can cause complications such as blindness, heart disease, kidney problems, nerve damage and erectile dysfunction (did that one get your attention?).
For myself, I like to look at diabetes like an engine. A normal working pancreas is running on all cylinders – much like an engine on gasoline, it burns sugar as fuel. A Type-1 diabetic – well their pancreas is dead and does not burn any sugar, insulin is used as a substitute to manage glucose control. With Type-2 diabetes, look at it as our pancreas is getting lazy. In my case, my pancreas is working at about 30% – or back to my engine analogy running on three of eight cylinders. The engine sounds like crap, however, it will still get us from point A to point B – just don’t count on it do it well or pretty. Overall, I blame my Crohn’s – yes, Type-2 diabetes does run in my family. My mom was diagnosed in her late fifties, her uncle around the same age – however for me, at 38, I was a bit ahead of the curve. At the same time, I have had the fun experience of having pancreatitis (inflexion in the pancreas) on two occasions that probably beat the pulp out of my pancreas. I suppose it could be worse – I could have easily ended up as a Type-1 diabetic.
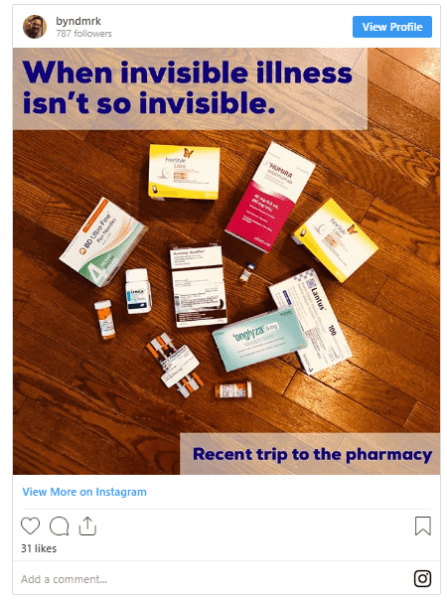
OCTOBER 2018: The last few months have been interesting and my diabetes has been kicking my butt. Lethargic, my A1C shooting up, rarely a blood sugar reading below 16 (300 mg/dl), and my c=peptide tanking. For the time being (I am being optimistic) a full fast acting regiment of insulin before every meal along with the remainder of my diabetes pills and injections. I will be sure to check in again soon with an update.
Life as a Diabetic with Crohn’s
It is always fun going back and reading some of my older blog posts. It is 2017, seven years after I originally wrote this post. It is incredible how quickly time flies. Today I am an insulin-dependant Type-2 diabetic and a Crohnie and the best part, most people would not know about either. I exercise (run and the gym), I still enjoy ice-cream and milkshakes, and still have terrible glucose days, however, my A1C or HBA1c is typically below 7.
The A1C test is a common blood test used to diagnose type 1 and type 2 diabetes and then to gauge how well you’re managing your diabetes. The A1C test goes by many other names, including glycated hemoglobin, glycosylated hemoglobin, hemoglobin A1C and HbA1c.
The A1C test result reflects your average blood sugar level for the past two to three months. Specifically, the A1C test measures what percentage of your hemoglobin — a protein in red blood cells that carries oxygen — is coated with sugar (glycated). The higher your A1C level, the poorer your blood sugar control and the higher your risk of diabetes complications. Typically an A1C of less then 7 is considered good glucose management.
Food and being a Crohn’s patient has always been a challenge – high finer, low glucose is always best for diabetics. However, high fibre may not necessarily work for Crohn’s patients all of the time. This is particularly important when we are fighting a flareup. Although I spend most of my life balancing my Crohn’s on pillars of Methotrexate and Humira when I have had to fall back to Prednisone my glucose levels have skyrocketed. However, following these basic rules sets great habits no matter how our other chronic disease is behaving and, knock on wood, life for me seems pretty “normal” – I know it is a relative word.
| Tips | Reasons |
|---|---|
| Eat three meals per day at regular times and space meals no more than six hours apart. You may benefit from a healthy snack. | Eating at regular times helps your body control blood glucose (sugar) levels. |
| Limit sugars and sweets such as sugar, regular pop, desserts, candies, jam and honey. | The more sugar you eat, the higher your blood glucose will be. Artificial sweeteners can be useful. |
| Limit the amount of high-fat food you eat such as fried foods, chips and pastries. | High-fat foods may cause you to gain weight. A healthy weight helps with blood glucose (sugar) control and is healthier for your heart. |
| Eat more high-fibre foods such as whole-grain bread and cereals, lentils, dried beans and peas, brown rice, vegetables and fruits. | Foods high in fibre may help you feel full and may lower blood glucose (sugar) and cholesterol levels. |
| If you are thirsty, drink water. | Drinking regular pop and fruit juice will raise your blood glucose (sugar). |
| Add physical activity to your life. – No excuses here, I live off of Methotrexate and Humira. I have bad days / weeks like everyone else however, exercise does wonders. | Regular physical activity will improve your blood glucose (sugar) control. |
Source: https://www.diabetes.ca/diabetes-and-you/healthy-living-resources/diet-nutrition/basic-meal-planning
MARCH 2020: Sadly optimism doesn’t win with diabetes, 18 months later I officially consider myself an insulin-dependant Type-2 diabetic. Life could be worse? After all, how many people can stand up and proudly say they have not one but two chronic diseases – LOL
Eat Right Ontario
For those like myself that live in Ontario, Canada – EatRight Ontario (ERO) is a free service that connects residents of Ontario to the trusted advice of a Registered Dietitian to help you make healthier food choices and answer your nutrition questions.
Whether you are a parent, consumer, health professional or community leader, here are the three easy ways to reach a Registered Dietitian. Check out their website at www.eatrightontario.ca or:
- Call this toll-free number: 1-877-510-510-2
- Email the Email a Dietitian service
- Use this website to read healthy eating articles, watch videos, find recipes and explore interactive tools to help you with menu planning and portion sizes and setting goals
Recent Research Study on Crohn’s and Diabetes
Is there an association between Crohn’s Disease. Inflammatory Bowel Disease, and Diabetes? A quick literature and journal review found some interesting results.
Inflammatory Bowel Disease Increases Risk of Type 2 Diabetes in a Nationwide Cohort Study
Recently, two Danish researchers, found that there is a relationship between Irritable Bowel Disease (IBD) and Type-2 Diabetes.
Researchers explored the long-term risk for type 2 diabetes in patients with IBD by performing a nationwide, population-based cohort study in Demark. They analyzed data comprising more than 6 million individuals to compare the risk for diabetes between patients diagnosed with UC (n = 44,915) or CD (n = 20,265) with individuals without IBD between 1977 and 2014. Over the course of 732,072 person-years of follow-up, 3,436 patients with IBD developed type 2 diabetes vs. 2,224 expected cases (standardized incidence ratio [SIR] = 1.54; 95% CI, 1.49–1.6). The risk was increased for both patients with UC and patients with CD, as well as in women and in men.
Although the risk for diabetes was highest in the first year after IBD diagnosis (SIR = 4.48; 95% CI, 1.5–1.65), it remained increased for 20 or more years (SIR = 1.26; 95% CI, 1.16–1.38). Patients who were diagnosed between 2003 and 2014 were at higher risk compared with patients diagnosed in the two other time cohorts; 1977 to 1988 and 1989 through 2002.
“The risk persisted long-term, was not explained by detection bias or corticosteroid exposure and was present in both CD and UC patients,” Jess and colleagues wrote. “The risk was particularly high in patients diagnosed in the new millennium, hence warranting further investigations into the impact of IBD treatments on diabetes risk.
Read the article here: Jess T, et al. Clin Gastroenterol Hepatol. 2019;doi:10.1016/j.cgh.2019.07.052.
Increased Risk of Diabetes in Inflammatory Bowel Disease Patients: A Nationwide Population-Based Study in Korea
A cohort study out of Inflammatory Bowel Disease Patients in South Korea published similar results to the Danish study.
Newly diagnosed diabetics were identified using International Classification of Disease (ICD-10) codes and the prescription of anti-diabetic medication by the end of the follow-up period (2016) was investigated.
The study found that the during a mean follow-up of 5.1 years, the incidence of diabetes in patients with IBD was significantly higher compared with controls after adjusting for serum glucose levels and steroid use (23.19 vs. 22.02 per 1000 person-years; hazard ratio (HR), 1.135; 95% confidence interval (CI), 1.048–1.228). The risk of diabetes was significantly higher in patients with CD (HR, 1.677; 95% CI, 1.408–1.997), but not in UC (HR, 1.061; 95% CI, 0.973–1.156). The effect of IBD on the development of diabetes was significantly more prominent in younger patients (p < 0.001). Patients with CD are at a higher risk of diabetes. Regular monitoring for diabetes is recommended, even in younger CD patients who do not use steroid medication.
Read the article here: J Clin Med. 2019 Aug; 8(8): 1191. Published online 2019 Aug 8. doi: 10.3390/jcm8081191
What is your Crohn’s and Diabetes Story – Comment Below?
I know most of the readers of this article came here looking for answers. I wish I had some definite answers for you. For me, my Crohn’s came first, followed by diabetes. What about you?
Notes: Edited September 25, 2017, 2020. Originally published April 1, 2010.


